 During these stressful times of COVID-19, it’s important that science guide our understanding of the condition, it’s treatments, and a future vaccine. At the same time, we should also turn to science to help us make sense of our psychological and emotional state, and the steps we can take to mitigate behavioral health challenges and enhance our resilience to what is turning out to be a marathon and not a sprint.
During these stressful times of COVID-19, it’s important that science guide our understanding of the condition, it’s treatments, and a future vaccine. At the same time, we should also turn to science to help us make sense of our psychological and emotional state, and the steps we can take to mitigate behavioral health challenges and enhance our resilience to what is turning out to be a marathon and not a sprint.
Continuous Traumatic Stress (CTS)
A useful way to think about how the pandemic is influencing our daily mental health, is the concept of continuous traumatic stress (CTS). It was first described in 1987 by a clinical team working with South African victims of state oppression who had endured torture, imprisonment, and the fear of death. Despite getting therapy, the victims faced a high likelihood that the traumas would continue, so the “post” in post-traumatic stress disorder was not really accurate. This new phenomenon was characterized by:
- Non-pathologizing language and a recognition that anyone going through such stress would have symptoms
- Real, life-threatening stress differentiated from everyday chronic stress
- A future-focus rather than trauma in the past, like with PTSD
- Threats that are largely faceless, unpredictable, and impact society in pervasive and significant ways
- A preoccupation with future safety and hypervigilance around accurately assessing future risks
- The absence of protections from future traumatic stress, which often includes a breakdown of community, law and order, and a predictable functioning society
Add to COVID-19 the stress and trauma from climate change (wildfires, smoke, hurricanes), racial injustice, hunger, poverty, (un)availability of healthcare, and contentious politics, and CTS reasonably describes our present state for some time to come.
Behavioral Health Toll
While we all are exposed to CTS, our individual responses will vary. In a recent study published in Science Advances, researchers utilized an existing nationally representative data set (n=6,514) to compare mental health pre and post-COVID-19. They conducted the survey in three waves between 3/18/20 and 4/18/20 and noted that when the first wave of data was collected there were 9,415 positive cases and 190 deaths in the U.S., but by the final wave the total positives for COVID-19 rose to 124,163 and about 3,500 deaths. And with each successive wave of data collection, they noted increased symptoms of stress and depression.
The strongest predictor of depressive symptoms was having a pre-COVID-19 mental health diagnosis. Also, loss of a job, decreased wages, and experiencing a shortage of necessities (e.g., food, toilet paper) not surprisingly increased both acute stress and depression. Among the most revealing findings was that “daily hours of pandemic-related media exposure, increases in daily media use, and exposure to conflicting information in the news media all predicted acute stress and depressive symptoms (p. 3).”
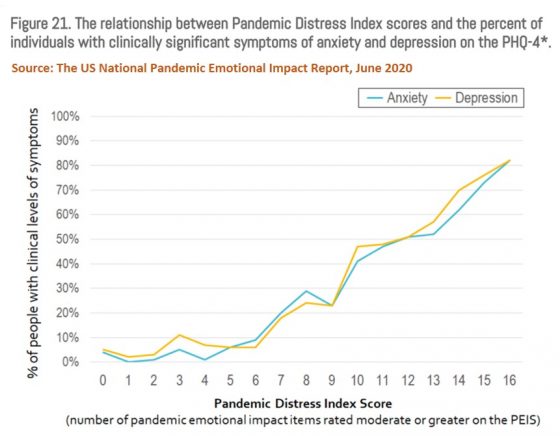 We also know from the ongoing Household Pulse Survey conducted by the CDC’s National Center for Health Statistics and the Census Bureau, and the U.S. National Pandemic Emotional Impact Report (June 2020) collaboratively done by researchers at Beth Israel Deaconess Medical Center, Massachusetts General Hospital, and the University of North Carolina at Chapel Hill School of Medicine, that symptoms of anxiety and depressive disorders have risen precipitously throughout the U.S. since the emergence of COVID-19.
We also know from the ongoing Household Pulse Survey conducted by the CDC’s National Center for Health Statistics and the Census Bureau, and the U.S. National Pandemic Emotional Impact Report (June 2020) collaboratively done by researchers at Beth Israel Deaconess Medical Center, Massachusetts General Hospital, and the University of North Carolina at Chapel Hill School of Medicine, that symptoms of anxiety and depressive disorders have risen precipitously throughout the U.S. since the emergence of COVID-19.
It’s also not surprising that addiction-related challenges have increased significantly. A recent paper on the intersection of substance use disorders and COVID-19 details how the pandemic has disproportionately impacted those who struggle with addiction. Quarantines have exacerbated isolation and loneliness, mental and physical co-morbidities, and withdrawal symptoms. The convergence of the pandemic with the opioid epidemic has resulted in a 61% increase in overdose submissions to the Overdose Detection Mapping Application Program while treatment budgets have significantly decreased.
So, what are we to make of the obvious fact that being in the midst of a pandemic is not particularly good on our behavioral health?
Four Likely Responses to COVID-19
Dr. George Bonnano and his colleagues have been studying how people respond to loss, trauma, and life threatening experiences for over two decades. His insightful work has revealed four trajectories or paths people will likely follow during and after COVID-19:
- Path of Resilience: Most people (~66%) will experience the path of resilience, which is characterized by an ability to maintain a relatively stable level of everyday functioning in the face of the pandemic. Most will adapt to new ways of remote working, shopping for groceries while wearing a mask, and staying connected with friends on Zoom or in small socially-distanced backyard gatherings. While psychological or emotional symptoms will occur, they’ll be sporadic, sub-clinical, and not have any lasting disruptive effect on life.
- Path of Recovery: A second group of folks (~21%) will take the path of recovery, experienced as a gradual return to normal functioning following the onset of more significant clinical symptoms in response to the pandemic. While in the midst of the symptoms, key to this path is getting the help necessary to recover versus staying stuck in anxiety and depression to the degree that the symptoms become chronic and more severe over time.
- Path of Chronic Symptoms: A third group (~11%) will struggle with clinical symptoms during and after the pandemic, often leading to the diagnosis of PTSD. This group is also the most likely to have a mental health diagnosis pre-COVID-19 and benefit from early identification and intervention.
- Path of Delayed Onset: A final group (~9%) will show less clinical symptoms during the pandemic, but then struggle more in its aftermath. This group is at risk for PTSD and symptoms becoming chronic if not addressed.
Note: Percentages for each path come from a review of 54 studies and do not total 100%. Check out this presentation on PTSD, Resilience, and Everything in Between by Dr. Bonnano to learn more about his work and these trajectories.
Because I was curious to know how we can tell which path people are on and how to maximize the number that experience resilience, I reached out to Dr. Bonnano to get his take. In short, he said “there is no simple way to measure the trajectories, unfortunately. However, you can still do things the way they’ve always been done, which is to simply measure adjustment (mental health, etc.) at a future time point and see if you can move the bar, or prevent the development of problems.”
7 Steps to Staying Healthy During a Pandemic
 Before jumping into what you can do to stay healthy, it’s important to acknowledge that each person’s path during COVID-19 will be influenced by a combination of individual and community-level factors. Some will face much greater adversity than others because of the color of their skin, where they live, a lack of community protections, and an inability to access economic and healthcare resources. Problems of racism, injustice, and poverty become even more pronounced during times of continuous traumatic stress, placing an extra burden on those most vulnerable. Engaging in the steps that follow can help mitigate the behavioral health consequences of this pandemic, but for those whose very survival is being tested daily, they also deserve and should have access to local, state, and federal resources.
Before jumping into what you can do to stay healthy, it’s important to acknowledge that each person’s path during COVID-19 will be influenced by a combination of individual and community-level factors. Some will face much greater adversity than others because of the color of their skin, where they live, a lack of community protections, and an inability to access economic and healthcare resources. Problems of racism, injustice, and poverty become even more pronounced during times of continuous traumatic stress, placing an extra burden on those most vulnerable. Engaging in the steps that follow can help mitigate the behavioral health consequences of this pandemic, but for those whose very survival is being tested daily, they also deserve and should have access to local, state, and federal resources.
Whatever path you happen to be on at this time, do your best to engage in the following seven steps to keep your sanity during this incredibly challenging time.
- Monitor your symptoms. Because the pandemic will continue to influence life in unique and pervasive ways for months (or years) to come, and your symptoms will vary over time, it’s hard to know objectively how much they are impacting your life without utilizing a valid and reliable assessment measure. Use this quick assessment tool (Depression, Anxiety & Stress Test) to measure your level of symptoms every few weeks. If you score in the moderate to high range and feel you would benefit from help, then reach out to your doctor or a behavioral health professional. If your scores are in the normal to mild range and you feel you are functioning fairly well, then keep monitoring your symptoms.
- Focus on the basics. The pandemic has led many to feeling like prisoners in their own homes, where sleep, work, exercise, and school routines have all been massively disrupted. The result has been a breakdown of normal boundaries between activities, days of the week, and even time spent with loved ones, contributing to feeling overwhelmed (for some) because trauma thrives on chaos. This means during the pandemic, it’s critical you stay focused on the basics in life, like getting solid sleep, eating a healthy diet, and exercising as best you can, even if that is just a daily 10-minute walk. The creative video Spaceship You offers helpful suggestions on how you can reestablish boundaries and stay healthy during these challenging times.
- Seek help if you’re not doing well. As was noted earlier, the strongest predictor of depressive symptoms was having a pre-COVID-19 mental health diagnosis. If you have struggled with mental health and/or addiction problems prior to the pandemic, lost a loved one, struggled personally with COVID-19 illness, became unemployed, or felt economic strain, then you likely have felt an added degree of distress and may be experiencing worsening symptoms. If so, don’t delay getting help. If you’ve never accessed treatment before, get referrals from family and friends who know you best, or start with your primary care physician or local community mental health provider. Most importantly, know that you are not alone right now and that reaching out is not a sign of weakness.
- Limit your consumption of pandemic-related media (and all screen time). In the study noted previously, researchers found that people were consuming an average of 7 hours of outbreak-related coverage daily. Add to this the additional hours spent engaging in screen time for other things and the evidence for how excessive screen time negatively impacts mental health, and it’s clear why managing your screen time is so important during the pandemic. It’s even more important in children and teens who are at greater risk for mental health problems the more technology they consume. Of course, this is easier said than done, and starts with the awareness of your screen time behavior and having the motivation to keep yourself in check. Today smartphones all have integrated tools to help you monitor and manage screen time, in addition to many apps that can also provide support.
 Stay connected. The popular TED Talk What Makes a Good Life? nicely summarizes decades of research from one of the longest-running studies of all time, and concludes that relationships are the holy grail to a good life. Unfortunately, the necessity for social (or physical) distancing during the pandemic has significantly decreased our interactions with family and friends. It’s been painful not seeing, hugging, or kissing our loved ones. Many have had to dramatically alter wedding, birthday, and travel plans. Perhaps the greatest suffering has been our inability to be with a loved one or friend when they are gravely ill or passing because of hospital restrictions. Yet during times of stress, it’s all the more critical we reach out and stay connected to those we care about by phone, through video-based platforms (e.g., Zoom, FaceTime, Skype, WhatsApp), and when possible, face-to-face using necessary precautions (e.g., physically distancing, wearing a mask, meeting outdoors). For those living with a partner and/or children, it’s critical to keep symptoms in check (see above) and mitigate relational damage (with professional help if necessary) that can be exacerbated by stress.
Stay connected. The popular TED Talk What Makes a Good Life? nicely summarizes decades of research from one of the longest-running studies of all time, and concludes that relationships are the holy grail to a good life. Unfortunately, the necessity for social (or physical) distancing during the pandemic has significantly decreased our interactions with family and friends. It’s been painful not seeing, hugging, or kissing our loved ones. Many have had to dramatically alter wedding, birthday, and travel plans. Perhaps the greatest suffering has been our inability to be with a loved one or friend when they are gravely ill or passing because of hospital restrictions. Yet during times of stress, it’s all the more critical we reach out and stay connected to those we care about by phone, through video-based platforms (e.g., Zoom, FaceTime, Skype, WhatsApp), and when possible, face-to-face using necessary precautions (e.g., physically distancing, wearing a mask, meeting outdoors). For those living with a partner and/or children, it’s critical to keep symptoms in check (see above) and mitigate relational damage (with professional help if necessary) that can be exacerbated by stress.- Create. While the downsides of COVID-19 are clear, the pandemic has resulted in some surprising upsides including animals coming out of hiding, cleaner air, and more time to smell the roses. For those who have felt overwhelmed by the treadmill of life, there is now an opportunity to reexamine what is most important and create a life more aligned with how you want to live. The process of creating anything is not something most of us have ever been taught, but creating is built into our DNA as humans. We all have natural talents and gifts that if not identified and nurtured, will contribute to a lack of meaning and feeling of aliveness. The pandemic has created an opportunity for you to engage your creative juices. By doing so, you harness a positive energy that can buffer negative feelings and support being on the path of resilience. Whether you turn to art, music, writing, building a business, tending a garden, evolving a new relationship, or deepening your connection with your personal faith, engaging your creativity is vital during this challenging time.
- Process your grief. COVID-19 has taken so much from us, and is poised to take even more if we fail to recognize the coming pandemic of unresolved grief. When feelings of unprocessed grief accumulate in the body, a wall is built around our emotional world to fend off reexperiencing overwhelming feelings from past loss. But the price we pay for not learning how to embrace grief is more suffering, because the wall that fends off grief also blocks our ability to truly feel alive. Kahil Gibran said, “The deeper that sorrow carves into your being, the more joy you can contain.” This is only true so long as you learn to feel your grief and not allow it to block the joy of life. For some this comes naturally, and yet for others, there is work to be done. Grief therapist and author, Francis Weller, offers a helpful framework for understanding and addressing grief in his book, The Wild Edge of Sorrow. Also check out his recently published collection of essays: In the Absence of the Ordinary.